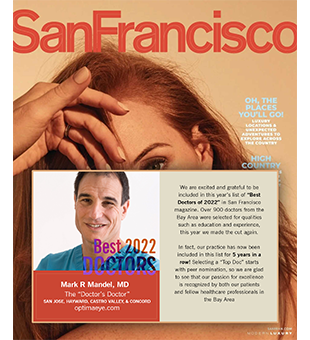
Offices in Hayward, Castro Valley, Concord, & San Jose
Learn what to expect during every stage of the LASIK procedure, from the moment you arrive at our office, to your recovery period.
Contact us today to schedule your FREE LASIK consultation!
Want to get LASIK laser eye surgery in the Bay Area? LASIK is a trusted surgical process that helps Dr. Mandel’s patients improve their vision, and reduce their need for glasses.
- Are you a LASIK Candidate?
- LASIK Overview
- Laser Surgery Expectations
- Femtosecond All-Laser LASIK Re-defined
- Wavefront Customized Treatment
- Why Choose Dr. Mandel
- LASIK Recovery
- Complications During the LASIK Procedure
- Post-Operative Complications and Side Effects of LASIK
- Answers to the Most Common Patient Concerns
- Printable LASIK Brochure