Offices in Hayward, Castro Valley, Concord & San Jose
Custom Eye Surgery with Wavefront Wave® EX 500
For years, excimer lasers have been used for LASIK and PRK, to correct “lower order” abnormalities (aberrations), such as nearsightedness, farsightedness, and astigmatism. However, other visual distortions, called “higher order aberrations,” can be responsible for decreasing the overall quality of your vision.
These imperfections in your eye’s optical system may affect the clarity of your vision and how well you see at night or in low light conditions. Higher order aberrations are more apparent when the pupil is large and can cause glare, halos, and other unpleasant visual effects.
Unless these higher order aberrations are kept to a minimum, the quality of your vision after your laser treatment may not be ideal, even if you have measurable vision of 20/20 in the exam room.
Contact us today to schedule your FREE LASIK consultation!
With Wavefront laser treatment, hundreds of individual sites on the cornea are treated to minimize higher order aberrations, thereby diminishing glare, halos, starbursts, and decreased contrast sensitivity. The ALLEGRETTO WAVE® EX 500 customizes every treatment based on the patient’s individual prescription and the shape of their cornea. The Wavefront Optimized™ treatment considers the unique curvature and biomechanics of the eye to preserve the quality of vision by inducing fewer distortions that can cause glare and halos at night.
Allegretto Wavelight
We use the Allegretto Wavelight EX 500 wavefront and pupil/eye tracking laser with the latest software and hardware upgrade.
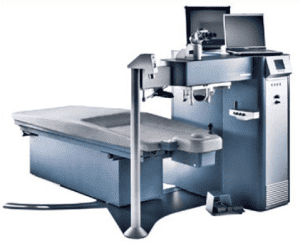
The excimer laser beam is centered on the eye in a team approach between the patient and our specialists . Specifically, the patient is coached and encouraged to maintain fixation on a blinking light and the surgeon, using a joystick and subtle manipulations of the patient’s head, maintains fixation and centration on the patient’s pupil.
Although most patients are concerned that they will be unable to fixate on the light, in reality most people fixate extremely well. However, there are some patients who have a difficult time fixating on the light. Additionally, there are some medical conditions of the eye such as nystagmus, which prevent the patient from fixating.
We use the latest technology to ensure your safety by employing only lasers with active tracking mechanisms, so there are no worries about slight eye movement. We have been thrilled with the results of the Allegretto laser tracking system. If, for no other reason than this system has been very useful in allaying anxiety of patients afraid that they will not be able to “watch the light” during laser treatment.
Complications During the LASIK Procedure
Complications during the operation are uncommon and include the following: inability to seat the suction ring and/or inadequate suction, incomplete femtosecond laser pass, irregular flap or tearing of the flap. These may prevent us from performing LASIK or result in an inadequate flap requiring the procedure to be rescheduled at another time in the future. This could result in astigmatism or inadequate correction. Less common is the creation of a free unhinged cap (which requires suturing back in place) or loss of the flap (exceptionally rare). If the flap is lost, a PRK or possibly a partial or full-thickness corneal transplant would be required weeks to months following the flap loss. Vision without glasses or contacts is generally poor following these complications. It is theoretically possible that LASIK could result in blindness from disruption of the blood supply to the optic nerve or retina.
Possible excimer complications include decentered ablation (the treatment area is decentered), or improper focus by the patient on the target device. These can cause under corrections, overcorrections, and astigmatism, which could require additional surgical corrections (laser or astigmatic keratotomy) and quite possibly result in loss of best correctable visual acuity, glare, ghost images, double vision, and halos, which cannot be corrected. Generally, a decentered ablation cannot be corrected surgically and results in the need to wear a gas permeable or scleral contact lens.
Post-Operative Complications and Side Effects of LASIK
Pain: During the procedure, LASIK is basically painless. Topical anesthetic drops provide excellent anesthesia. No injections are required. Patients experience pressure when the suction ring is applied. This lasts for approximately 60 seconds. There is usually minimal to no post-operative pain following LASIK. Some initial soreness may occur due to the suction ring. A feeling of scratchiness may be experienced the first night and will usually be gone by the following morning.
Subconjunctival Hemorrhages: Small broken vessels on the white of the eye due to the suction ring are common. They cause no problem and clear within two weeks.
Light Sensitivity: Your eyes will be somewhat light sensitive, and you may experience glare during the day and at night during the first few months.
Overcorrection, under-correction or induced astigmatism: There can be a mild overcorrection, under-correction or astigmatism initially after almost all refractive surgeries. This will usually diminish over the following weeks to months. Significant permanent overcorrection, under-correction or astigmatism can be corrected with glasses or contact lenses or a laser “touch-up.”
Ghost Images and Double Vision from One Eye: This is due to the surface of the cornea healing with a “wavy” configuration or from the induction of “higher order aberrations.” This can also give rise to distortion of images and a decrease in spectacle correctable vision, glare, halos, starbursts and decreased contrast vision. Many cases of visual distortion resolve within a year. However, if it does not, then these symptoms can sometimes be diminished by the use of a gas permeable or scleral contact lens. While the lens is in place, the distortion and ghost images will not be as noticeable. However, when the lens is removed, the distortion and ghost images will reappear. A very small number of patients may be required to wear gas permeable or scleral contact lenses full-time following LASIK in order to achieve their very best vision and to diminish distortions.
Sometimes visual distortions can be caused by a LASIK-induced “dry eye.” If this is the case, with the use of non-preserved artificial tear drops, oral omega 3, plugs in the tear drains, and possibly Restasis or Xiidra eye drops, and/or “serum tears.” Most cases of post-LASIK “dry eye” resolve within 12 to 18 months.
Folds (like the striations seen just before tearing a piece of cellophane off of a roll) occur in about 5% of flaps in people with high amounts of myopia (6.00 diopters or more), and occasionally lower myopes who require large zones of treatment. Most of the time the folds do not cause symptoms, but occasionally they can result in distorted vision, decreased vision, or a decrease in contrast appreciation. Additionally, patients may notice starbursts, glare and halos at night. If patients have symptoms from microfolds, the flaps may be lifted and an attempt to “iron-out” the folds undertaken. However, in some cases, the folds cannot be “ironed out” and patients may have persistent symptoms and be required to wear a gas permeable or scleral contact lens to decrease these symptoms.
Night Vision: Glare, halos, and starbursts around lights are very common initially following LASIK. These symptoms may last 6 to 12 months. They generally diminish significantly by one year but may persist. A decrease in night vision quality (contrast) may be noticed. Patients occasionally require night driving glasses following refractive surgery.
Enhancement Procedures: Enhancements or touch-ups may be necessary following LASIK. Enhancements may be requested due to regression, under correction, overcorrection or induced astigmatism. In the milder myopic corrections (under -4.00 diopters), enhancements are usually needed in less than 2% of cases. In moderate myopic corrections (-4.00 to -6.00 diopters), the enhancement rate is approximately 5%. The higher myopic corrections (-6.00 diopters and above) will have a greater percentage of enhancements. The higher the myopia, astigmatism, or hyperopia, the higher the enhancement rate. When astigmatism correction is combined with myopic or hyperopic correction, the need for enhancements is slightly increased. This is especially true with astigmatism corrections over 3.00 diopters. Occasionally, astigmatism will be created by the LASIK or laser procedure where none existed pre-operatively. In most (but not all) cases, this induced (regular) astigmatism can be reduced with an astigmatic keratotomy or a laser touch-up procedure. The enhancement rate for higher amounts of hyperopia/farsightedness (+4.00 and above) is about 20%. Also, patients who are long-term hard contact lens wearers (RGP lenses) will have a higher enhancement rate.
Infection: This can be a serious complication, but fortunately is extremely rare in all types of refractive surgery. Most can be treated effectively with antibiotics, but in the extremely rare case, vision or the eye could be permanently lost.
Permanent Decrease in Vision: All refractive surgery results in some decrease in what is known as contrast vision – the ability to discern subtle shades of gray. This is a qualitative measurement of vision. Clinically, some patients will notice a decrease in the quality of their night vision. Rarely is this a significant decrease.
The chance of reduced correctable (with glasses) vision (greater than two eye chart lines of vision) is 0.5% to 2.0%. It is highest in myopic corrections above -7.00 diopters and hyperopic corrections above +4.00 diopters, and in cases of high astigmatism above 4.00 diopters. The chance of extreme or total loss of vision is exceedingly low with LASIK. The potential causes are severe infections, corneal scarring, and optic nerve or blood vessel damage or retinal detachment.
Rarely, following LASIK, the cornea progressively becomes thinner and steeper. This is called “ectasia” and is essentially the development of (or progression of) pre-existing but sub-clinical “keratoconus.” If this occurs, patients must wear gas permeable or scleral contact lenses or undergo additional surgery such as Intacs, with or without corneal cross-linking, or corneal transplantation.
Additional Post-Operative Complications: Material under the flap (usually of no consequence) rarely may have to be rinsed from underneath the flap. If the flap becomes dislocated, the flap may need to be lifted and repositioned. Epithelial in-growth is growth of the corneal surface epithelial cells beneath the flap. This requires lifting the flap and removing the epithelium. Melting of the cornea from epithelial in-growth is rare, but if occurs can be a serious problem. In-growth may require suturing (with or without gluing) of the flap if it reoccurs. Sterile white blood cell infiltration can occur beneath the flap (DLK or CTK). This is treated by increasing the frequency of the use of your topical cortisone drops. Occasionally the flap must be lifted to help treat DLK. Sometimes this inflammation can cause a poor visual result.
There are other possible complications and side effects, which are not mentioned because of their extreme rarity.
Fortunately, refractive surgery procedures are safe and effective, and complications are rare. However, like any operation, problems can occur, and patients must always weigh the risk and the benefits before undergoing surgery.
Answers to the Most Common Patient Concerns
Q: Is LASIK right for me?
A: If you are considering LASIK eye surgery, it means you are living with nearsightedness, farsightedness and/or astigmatism, and probably currently wear glasses or contact lenses. LASIK is a great way to reduce your dependence on, or completely free yourself from, corrective lenses. It may be especially appealing because of your profession or lifestyle. It could be that you cannot wear contact lenses and dislike the inconvenience of glasses, or you may just want to reduce the expense and hassle of glasses and contacts.
However, LASIK is not appropriate for everyone. There are several factors which determine the best candidate, including age, medical history, individual eye anatomy, and expectations. Each person is a unique case requiring individual evaluation.
No website can tell you for sure if you are a good candidate for LASIK. The only way to find out is to schedule a LASIK eligibility exam. Be prepared to talk about your medical history, and any current eye or general health conditions or medications. You will also discuss instructions and expectations for the procedure, recovery, and results. You will be given a comprehensive eye examination, including some tests especially tailored to evaluate whether your eyes are appropriate for the corrective surgery. From the results of this exam, the doctor can work with you to decide if LASIK is the right choice for you.
Q: Is LASIK safe?
A: It is important to realize that, like any surgery, LASIK is not without risk. However, major complications are extremely rare. Minor complications occasionally occur, such as dry eye, and halos or glare around lights at night. However, such problems are uncommon, are often treatable, and will usually reduce or disappear within months of the surgery.
Q: Does LASIK hurt?
A: There is no pain associated with the LASIK procedure. Local anesthesia is used on the cornea, which is administered through eyedrops. Some patients may experience mild discomfort or pressure. After the procedure, patients may experience minor irritation in the eye for about four to six hours.
Q: Is LASIK guaranteed to eliminate my need for glasses or contacts?
A: Many people achieve 20/20 vision or better after undergoing LASIK eye surgery. Although patients experience an improvement in their vision, some may still need to wear corrective lenses for certain tasks, though generally the necessary power of correction will be smaller than before.
The result of the LASIK procedure is also influenced by the amount of correction needed. Patients within a few diopters of 20/20 vision most often achieve sufficient results after undergoing LASIK that they no longer require corrective lenses. Patients with a higher error, especially those who are extremely nearsighted or farsighted or who have large amounts of astigmatism, sometimes will still require corrective lenses after the surgery, though their prescription will be greatly reduced. However, in most cases, if full correction is not achieved, an enhancement or “touch-up” procedure can be performed to significantly reduce or eliminate the need for glasses.
Q: What Is Laser Vision Correction?
A: Laser vision correction encompasses several procedures, (LASIK and PRK) which utilize the wavefront excimer laser to correct nearsightedness, farsightedness and astigmatism. During the treatment, the laser’s cool ultraviolet light removes a small amount of corneal tissue to reshape the corneal surface in order to allow light to be more sharply focused onto the retina, thereby improving vision.
Patients considering laser vision correction should have a stable refraction for at least one year. After the procedure, eyeglass correction or contact lenses for distance vision will generally not be required. If you are in the age range where bifocals or “readers” are normally required for close vision (40+ years of age), you will need reading glasses following the procedure. This condition is known as presbyopia and is part of the natural aging process. Some patients elect to have monovision. This is when one eye is adjusted for near (reading) vision and the other is adjusted for full distance.
After 40 years old, monovision will allow most patients to see well at distance and near. For some monovision patients, glasses may be required for night driving.
Schedule a Consultation Today
Wavefront LASIK is one of the most advanced laser technologies currently available. Dr. Mark R. Mandel and the team at OPTIMA Eye are pleased to offer this sophisticated treatment to patients throughout San Jose and the East Bay Area. If you would like to learn more about Wavefront LASIK, or would like to schedule a consultation, contact us today at 877-210-2020 ext. 3. OPTIMA has convenient locations in San Jose, Hayward, Castro Valley and Concord, CA.